
Delirium vs. Dementia: What's the Difference?

If your loved one is suddenly displaying signs of confusion or having emotional outbursts, you may be worried that they have dementia, a permanent and progressive condition of the brain that results in memory impairments. However, it’s possible they are showing signs of delirium, a temporary, abnormal mental state that causes confusion.
Delirium and dementia symptoms can be similar and are often mistaken for each other, so it’s important to learn about delirium, dementia, and how you can distinguish between the two.
Let our care assessment guide you
Our free tool provides options, advice, and next steps based on your unique situation.
Key Takeaways
- Confusion doesn’t always equal dementia. Confusion is an overlapping symptom of dementia and delirium, often causing people to mistake one for the other.
- Delirium can be caused by many factors Alcohol or drug intoxication, hospitalization, and prescription medications are common contributing factors to delirium.
- Dementia patients can also experience delirium. Physical brain changes associated with dementia put dementia patients at a risk for experiencing delirium.
- Delirium and dementia are diagnosed by a doctor. If you’re not sure what’s causing your loved one’s confusion, a doctor can perform a series of cognitive tests to properly diagnose symptoms as delirium or dementia.
What is the difference between delirium and dementia?

Delirium is a mental state of impaired attention, thinking ability, and alertness. Delirium is not a disease in and of itself. It is a term used to describe mental confusion resulting from different conditions.[01]
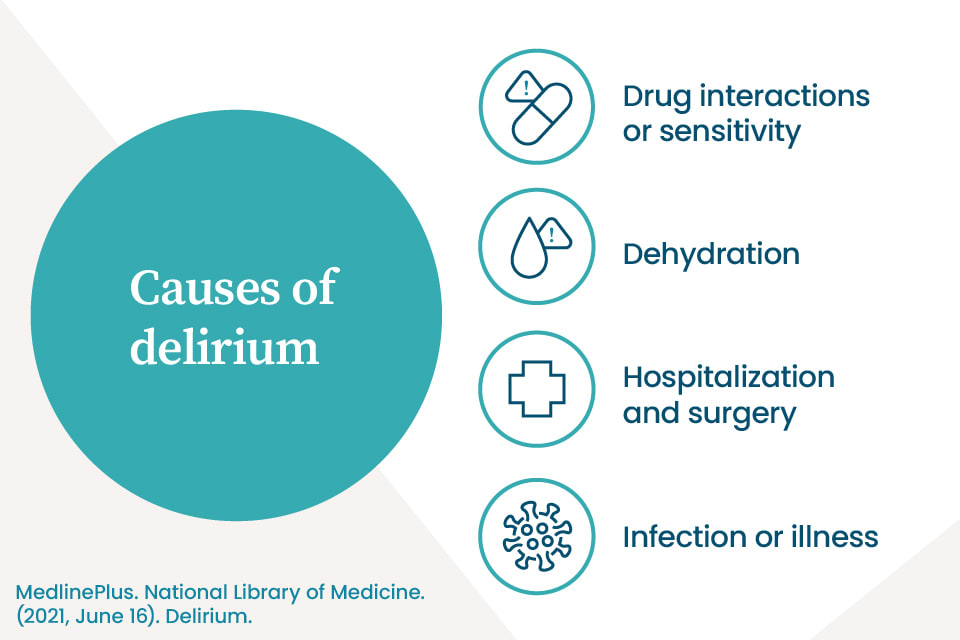
The following medical conditions and outcomes have all been linked to delirium [02]:
- Chronic illness and infections
- Hospitalizations [03]
- Medication interactions and side effects
- Dehydration
- Organ failure [04]
- Brain cancer and cancer treatments {citation:5}}
- Head injuries [06]
- Alcohol or drug intoxication
Dementia, on the other hand, is a condition where physical, memory-impairing changes occur in the brain. Dementia patients commonly lose their ability to remember, think clearly, and make decisions, and the result is a significant disruption of daily life. Risk factors for dementia include age, genetics, race, poor heart health, and traumatic brain injuries.[07]
Three major differences between delirium and dementia include the onset of the condition, how long it lasts, and a few key symptoms. Keep an eye out for how symptoms develop with delirium versus dementia.
Delirium symptoms typically:
- Begin suddenly and develop quickly
- Have a defined starting point
- Are temporary and reversible
- Cause difficulty with attention
- Cause slow, slurred speech during episodes
Dementia symptoms typically:
- Begin gradually and progress over time
- Have an unclear starting point
- Are permanent and worsen as the disease progresses
- Make it difficult to remember recent events
- Include speech problems, such as difficulty putting thoughts into words, inability to remember common words, and the repetition of words and phrases
The difference between delirium and dementia can be difficult to pinpoint. Symptoms often overlap, causing difficulties in diagnosis. While only a doctor can tell what’s causing your loved one’s condition, you can track and compare symptoms to help a doctor identify the problem.
Let our care assessment guide you
Our free tool provides options, advice, and next steps based on your unique situation.
What are the different symptoms of delirium and dementia?
The symptoms of delirium and dementia often get mixed up. However, some key differences can help you distinguish between the two. Take a look at the lists below to get a better understanding of the differences between delirium and dementia.
Symptoms of delirium
Although anyone can experience delirium, this mental disturbance is more common in older, hospitalized patients, affecting nearly 30% of them. The risk is even higher in patients who’ve had surgery, varying from 10% to greater than 50%.[02]
Delirium symptoms can include:
- Confusion
- Altered levels of consciousness
- Disrupted sleep patterns
- Emotional changes, especially anger, agitation, and depression
- Hallucinations and delusions
- Trouble with concentration
Delirium symptoms usually indicate a serious problem that requires immediate medical attention, especially in older adults. Luckily, delirium is usually temporary and reversible. Once the cause of delirium is treated, most symptoms typically go away.
Symptoms of dementia
Dementia symptoms that overlap with delirium include confusion, agitation, and delusions, so be sure to note all symptoms in order to spot the differences.
Dementia symptoms can include [07]:
- Memory loss, poor judgment, and confusion
- Shortened attention span
- Difficulty with communication
- Wandering and getting lost in familiar places
- Inability to complete daily tasks independently
- Behavioral changes like agitation, apathy, and lack of empathy
- Impulsiveness
- Delusions and paranoia
- Loss of balance and difficulties with movement
Can someone who has dementia also experience delirium?

Yes, because the physical brain changes related to dementia puts one at a higher risk for experiencing delirium.[08] People with dementia can experience episodes of delirium, and it may even seem like they are experiencing a period of rapidly progressing dementia. Such an episode may be due to an illness or one of the other causes of delirium listed above. Until the cause of the delirium is addressed, it may appear that you loved one’s dementia is rapidly worsening.
If your loved one sees a new health care professional during the onset of these new symptoms, it may be hard for them to distinguish between delirium and dementia because they don’t know how your loved one typically behaves.
For example, it can be especially hard to distinguish Lewy body dementia from delirium, as visual hallucinations, a key indicator of delirium, are also common in Lewy body dementia. For this and many reasons, tracking your loved one’s symptoms for their new doctor becomes critical to a proper diagnosis.
How is delirium diagnosed?
A delirium diagnosis is made after reviewing clinical history, notes from behavioral observations, and the results of cognitive tests. Doctors typically use a cognitive test called the 4AT test, in which they measure the following in a patient [09]:
- Alertness. Observes whether the patient is drowsy or agitated.
- Awareness. Identifies if a patient knows their whereabouts, the time, date, etc.
- Attention. Checks their ability to hold attention to a conversation, topics, etc.
- Acute or fluctuating changes. Identifies whether symptoms are sudden, if they come and go, etc.
If your loved one’s doctor suspects dementia, they may use more advanced cognitive assessments — such as the Mini-Mental State Exam (MMSE) or the Mini-Cog test — to assess your loved one’s cognitive abilities.[10]

Talk with a Senior Living Advisor
Our advisors help 300,000 families each year find the right senior care for their loved ones.
How can you help a loved one who is experiencing delirium?
It’s important to take notes of your loved one’s behavior so you can report changes to their doctor and quickly catch episodes of delirium. To help your loved one, be sure to remain an active part of their medical care:
- Stay connected. Check in with your elderly loved one often. If you don’t live nearby, use technology to stay in touch and check on their health and well-being.
- Speak up. If your loved one is not acting quite like their usual self, let their doctor know. Discuss any subtle changes, unusual symptoms, or behavioral changes you notice, even if you’re not sure they’re related. And, always bring a list of all of your loved one’s current medications to their appointments.
- Seek immediate care. If you notice a sudden difference in your senior’s mental state or behavior, it’s important to seek medical care right away.
Although delirium symptoms usually fade after the cause of delirium is addressed, it may take some time for your loved one to fully recover. During the aftermath of a delirium episode, your loved one may experience health issues or difficulty with readjusting to their lifestyle.
To help them recover and remain healthy, it’s important to come up with a long-term care plan. Consider living together for a while, so you can assist with their activities of daily living and foster a healthy lifestyle.
If that’s not a viable option, you can also seek help from an in-home care aide or even take advantage of respite care at a local assisted living facility. Reach out to one of A Place for Mom’s Senior Living Advisors. They can help you find local care options tailored to you and your loved one’s specific needs.
Senior living options in all states
The information contained on this page is for informational purposes only and is not intended to constitute medical, legal or financial advice or create a professional relationship between A Place for Mom and the reader. Always seek the advice of your health care provider, attorney or financial advisor with respect to any particular matter, and do not act or refrain from acting on the basis of anything you have read on this site. Links to third-party websites are only for the convenience of the reader; A Place for Mom does not endorse the contents of the third-party sites.
Make the best senior care decision
Make the best senior care decision